Understanding Maternal Cardiac Arrest
Cardiac arrest during pregnancy is rare but serious. According to the American Heart Association, maternal cardiac arrest occurs in approximately 1 in 9,000 hospital deliveries. Recent studies show this rate may be higher than previously estimated.
The challenge is clear. You’re dealing with two patients. The mother and her unborn child both need immediate help.

Common Causes of Cardiac Arrest in Pregnant Women
Several factors can trigger maternal cardiac arrest:
- Pre-eclampsia and eclampsia – High blood pressure and seizures during pregnancy
- Severe bleeding (hemorrhage) – Accounts for about one-third of cases
- Sepsis (infection) – Causes nearly half of all maternal arrests
- Pulmonary embolism – Blood clots blocking lung arteries
- Amniotic fluid embolism – Rare but life-threatening condition
- Heart conditions – Arrhythmia or valve problems
- Cardiovascular complications – Underlying heart disease
Can You Perform CPR on a Pregnant Woman?
Yes, you absolutely can and should perform CPR on a pregnant woman.
The American Heart Association makes this clear. CPR and AED use are safe for pregnant women. Not providing these life-saving measures reduces survival rates for both mother and fetus.
Many people hesitate. They worry about harming the baby. This fear is understandable but misplaced. The greatest risk comes from doing nothing.
Why CPR is Critical for Pregnant Women
Pregnant women face unique risks during cardiac arrest. Their bodies already work harder. The fetus requires large amounts of oxygen from the mother. Women experience a 20% increase in oxygen consumption during pregnancy.
Without immediate CPR, both lives are at risk. Brain damage can occur within minutes. Quick action saves lives.
What is True Regarding CPR and AED Use for a Pregnant Patient?
The 2025 American Heart Association Guidelines provide clear direction. CPR for pregnant women follows most standard protocols. However, key modifications improve outcomes.
Key Facts About CPR and AED Use in Pregnant Cardiac Arrest:
- Standard compression technique applies – Place hands on the center of the chest
- Same compression rate – 100-120 compressions per minute
- Same depth – At least 2 inches deep
- Rescue breaths are important – Provide 2 breaths after every 30 compressions
- Left lateral uterine displacement is crucial – Relieves pressure on major blood vessels
- AED use is safe – No evidence shows harm to the fetus from defibrillation
- Early defibrillation saves lives – Use the AED as soon as it arrives
The American Heart Association emphasizes high-quality CPR paired with uterine displacement. This combination improves blood flow to both mother and baby.
Critical Modifications for CPR on Pregnant Women
Performing CPR on a pregnant woman requires some adjustments. These modifications address the unique physiological changes of pregnancy.
Manual Left Lateral Uterine Displacement
After 20 weeks of pregnancy, the growing uterus can compress major blood vessels. This compression reduces blood return to the heart. It makes chest compressions less effective.
The solution: Manual left lateral uterine displacement.
A second rescuer should:
- Stand on the left side of the patient
- Place both hands on the right side of the uterus
- Push the uterus to the left
- Maintain this position throughout CPR
This simple action dramatically improves blood circulation during resuscitation.
Airway Management is Priority
According to the 2025 AHA Guidelines, airway management should be prioritized during pregnant cardiac arrest resuscitation. Pregnant women develop low oxygen levels more quickly than non-pregnant individuals.
Important considerations:
- Pregnancy causes airway changes
- Airways may be narrower due to swelling
- The risk of vomiting is higher
- 100% oxygen should be provided
- The most experienced provider should manage the airway
Hand Placement for Chest Compressions
Place your hands on the center of the chest. Use the same position as for non-pregnant patients. Previous recommendations suggested a higher placement. Current evidence does not support this change.
Keep compressions:
- At least 2 inches deep
- At a rate of 100-120 per minute
- With full chest recoil between compressions
- Continuous with minimal interruptions
Can You Use an AED on a Pregnant Woman?
Yes, using an AED on a pregnant woman is both safe and necessary.
This is one of the most important facts. AED use presents no harm to the fetus. The American Heart Association states clearly that defibrillation should not be delayed for pregnant patients.
Why AED Use is Safe in Pregnancy
Research shows no evidence that electrical shocks from an AED harm the fetus. The benefit of restarting the mother’s heart far outweighs any theoretical risk.
Every minute without defibrillation decreases survival chances by 7-10%. For pregnant women, this urgency is even greater. The fetus depends entirely on the mother’s circulation.
How to Use an AED on a Pregnant Woman
Follow standard AED procedures:
- Turn on the AED – Follow voice prompts
- Remove clothing – Expose the chest area
- Remove fetal monitors – If present, they could interfere with the shock
- Place AED pads – Use standard anterior-lateral placement
- Ensure no one touches the patient – Clear the area before shock delivery
- Deliver shock if advised – Press the shock button
- Resume CPR immediately – Start compressions right after the shock
Continue this cycle until emergency services arrive or the patient recovers.
Is Using an AED Safe in Pregnancy?
The evidence is overwhelming. AED use is not only safe but critical for maternal cardiac arrest.
What Studies Show
The American Heart Association’s scientific statements confirm AED safety. Multiple research studies and case reports demonstrate successful maternal resuscitation with defibrillation. No documented cases show fetal harm from appropriate defibrillation.
The 2020 and 2025 AHA Guidelines emphasize rapid automated defibrillation. This recommendation carries the highest level of evidence classification.
Survival Rates with Proper Intervention
Data shows encouraging results. Survival to hospital discharge after maternal cardiac arrest can reach 58.9%. This rate exceeds most arrest populations.
These numbers prove the effectiveness of immediate CPR and AED use in pregnant cardiac arrest situations. Proper training and quick response make the difference.
Step-by-Step Response to Pregnant Cardiac Arrest
When you encounter a pregnant woman who has collapsed, follow these steps:
1. Check for Responsiveness
- Tap her shoulders
- Shout to get a response
- Look for normal breathing
2. Call 911 Immediately
- Tell the dispatcher the patient is pregnant
- Request additional EMS resources
- Don’t delay calling for help
3. Begin CPR
- Place your hands on the center of the chest
- Start compressions at 100-120 per minute
- Push at least 2 inches deep
- Allow full chest recoil
4. Provide Rescue Breaths
- Give 2 breaths after every 30 compressions
- Ensure the chest rises with each breath
- Continue this cycle
5. Apply Left Lateral Uterine Displacement
- If a second rescuer is available
- Push the uterus to the left side
- Maintain throughout resuscitation
6. Use the AED as Soon as Available
- Turn on the device
- Remove fetal monitors if present
- Follow voice prompts exactly
- Deliver shock when advised
7. Continue Until Help Arrives
- Keep performing high-quality CPR
- Switch rescuers every 2 minutes if possible
- Don’t stop until professionals take over
The Importance of Professional CPR Training
Reading about CPR and AED use in pregnant cardiac arrest is helpful. However, hands-on training makes a real difference. Professional certification ensures you’re prepared for any emergency.
Why Get Certified?
- Build confidence – Practice on realistic training mannequins
- Learn proper technique – Expert instructors correct your form
- Stay current – Guidelines change as new research emerges
- Save lives – Your skills could save a mother and child
Certification programs cover:
- Standard CPR techniques
- Modifications for pregnant patients
- Proper AED operation
- Emergency response protocols
- Team coordination skills
Time-Sensitive Nature of Maternal Cardiac Arrest
Every minute matters. The 2025 AHA Guidelines emphasize urgent intervention. For pregnant patients, resuscitative delivery should be considered if spontaneous circulation doesn’t return within 4 minutes.
Team preparation should begin immediately with cardiac arrest recognition. Delivery of the fetus should be complete by 5 minutes if resuscitation efforts are unsuccessful.
This doesn’t mean giving up on the mother. Perimortem cesarean delivery actually improves maternal outcomes. It relieves pressure on blood vessels and returns blood back to circulation.
Special Considerations for Healthcare Providers
Healthcare professionals face additional responsibilities. The American Heart Association recommends a minimum of 4 staff members for BLS resuscitation of pregnant patients.
Multidisciplinary Response Required:
- Emergency response team
- Obstetric specialists
- Anesthesiology staff
- Neonatal team
- Equipment for emergency delivery
Hospitals must establish protocols. Regular drills ensure team readiness. Knowledge deficits and poor resuscitation skills contribute to poor outcomes.
Common Myths About CPR and AED Use in Pregnancy
Let’s address misconceptions:
Myth: “Chest compressions will harm the baby.”
Truth: Chest compressions help both mother and baby survive.
Myth: “AED shocks are dangerous during pregnancy.”
Truth: No evidence supports this concern. Defibrillation is safe and necessary.
Myth: “You should wait for medical professionals.”
Truth: Immediate action by bystanders dramatically improves survival.
Myth: “CPR techniques must be completely different.”
Truth: Most techniques remain the same with minor modifications.
Recovery and Post-Resuscitation Care
After successful resuscitation, pregnant patients require specialized care. The 2020 Guidelines recommend targeted temperature management for pregnant women recovering from cardiac arrest.
Healthcare providers should:
- Monitor the fetal heart rhythm continuously
- Watch for bradycardia and complications
- Provide intensive care management
- Coordinate between multiple specialties
For mothers who regain consciousness, positioning matters. Place the patient on her left side. This improves blood flow to both heart and fetus.
Take Action: Get CPR Certified Today
Understanding CPR and AED use in pregnant cardiac arrest is just the first step. Real preparedness comes from proper training and certification.
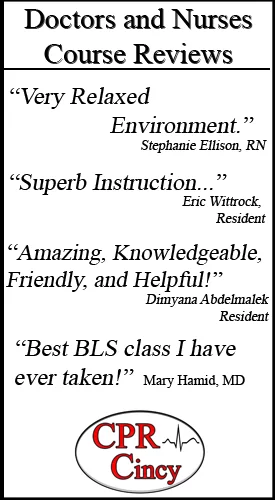
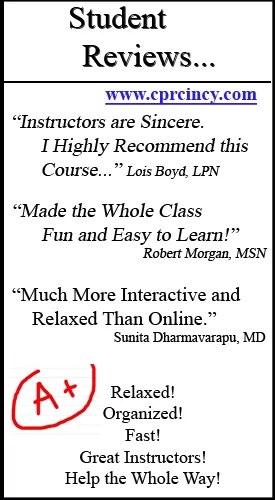
CPR Cincinnati offers comprehensive, hands-on training for all skill levels. As an American Heart Association training site, we provide:
- BLS for Healthcare Providers – Essential certification for medical professionals
- ACLS Certification – Advanced cardiac life support training
- PALS Training – Pediatric Advanced Life Support
- CPR and First Aid Courses – For community members and families
Our classes are:
- Stress-free and supportive
- Completely hands-on
- Taught by experienced instructors
- Aligned with current AHA guidelines
Whether you’re a healthcare provider or a concerned family member, our courses prepare you for real emergencies. Our training includes specific guidance on maternal cardiac arrest and other special situations.
Register for the AHA CPR Course in Cincinnati
Don’t wait for an emergency to wish you had training. Sign up for our AHA CPR course registration in Cincinnati today. Learn life-saving skills that could save a mother and her baby.
Join Our BLS Class in Cincinnati
Healthcare professionals need specialized training. Our BLS Class in Cincinnati covers advanced techniques for managing cardiac arrest in pregnant patients. You’ll practice modifications and team coordination.
Visit CPR Cincinnati to find course schedules and register. Invest a few hours now to gain skills that last a lifetime.
Conclusion
CPR and AED use in pregnant cardiac arrest saves lives. The evidence is clear. Immediate intervention with proper technique dramatically improves outcomes for both mother and baby.
Key takeaways:
- Yes, you can perform CPR on pregnant women
- AED use is completely safe during pregnancy
- Minor modifications improve effectiveness
- Left lateral uterine displacement is crucial
- Immediate action is essential
- Professional training builds confidence
Maternal cardiac arrest is rare. But when it happens, your knowledge and quick response make all the difference. Don’t hesitate. Don’t delay. Start CPR immediately. Use the AED without fear.
The best thing for the mother is the best thing for the baby. By saving one life, you save two.
Get certified. Stay prepared. Be ready to act when seconds count.
Frequently Asked Questions About CPR and AED Use in Pregnant Cardiac Arrest
1. Should I modify chest compression depth when performing CPR on a pregnant woman?
No, chest compression depth should remain the same. Push at least 2 inches deep in the center of the chest. Previous recommendations suggested shallower compressions, but current American Heart Association guidelines state that standard compression depth applies to pregnant patients. The key modification is adding left lateral uterine displacement while maintaining high-quality compressions at the proper depth and rate.
2. Will using an AED during pregnancy harm the unborn baby?
No, using an AED will not harm the baby. Multiple studies show no evidence that defibrillation shocks cause fetal harm. The American Heart Association clearly states that rapid automated defibrillation should be provided whenever indicated. The baby depends on the mother’s circulation for survival, so restarting the mother’s heart is the best way to protect both lives. Never delay AED use on a pregnant patient.
3. How is CPR on a pregnant woman different from standard CPR?
CPR on pregnant women follows most standard protocols with a few important modifications. The main differences include: adding manual left lateral uterine displacement to relieve pressure on major blood vessels, prioritizing airway management due to faster oxygen depletion, providing rescue breaths along with compressions (not just hands-only CPR), and being prepared for emergency delivery if resuscitation isn’t successful within 4-5 minutes. Hand placement, compression rate, and compression depth remain the same as standard CPR.
About CPR Cincinnati
CPR Cincinnati is an American Heart Association training site dedicated to providing high-quality, hands-on CPR and emergency cardiovascular care training. We offer initial certifications and renewals in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid courses. Our stress-free, practical approach ensures every student gains the confidence and skills needed to respond effectively in real emergencies.
Contact us today to register for our AHA CPR course in Cincinnati or join our next BLS Class in Cincinnati. Your training could save two lives.