Beyond CPR – The Critical Role of Reversible Causes
In the dynamic world of emergency medicine, Advanced Cardiovascular Life Support (ACLS) stands as a cornerstone for managing life-threatening cardiac emergencies. While immediate assessment for defibrillation and effective chest compressions are paramount, a crucial aspect of ACLS involves identifying and treating the underlying, reversible causes of cardiac arrest. These causes, often subtle yet critical, are encapsulated by a powerful mnemonic system: the “5 H’s and 5 T’s.” This article will delve specifically into the 5 T’s, providing a comprehensive overview of each condition, its recognition, and the vital treatment strategies that can dramatically improve patient outcomes. Understanding these T’s is not just about memorization; it’s about developing the clinical acumen to save lives when every second counts.
Unraveling the mystery of cardiac arrest means looking beyond the immediate lack of a pulse. Reversible causes are conditions that, if promptly identified and addressed, can restore spontaneous circulation and significantly enhance resuscitation success rates. Ignoring these underlying issues means that even the most perfect CPR may ultimately be futile. These H’s and T’s become especially critical when dealing with pulseless electrical activity (PEA) and asystole, where the heart’s electrical activity is present but insufficient to generate a pulse or absent. Recognizing these treatable conditions transforms cardiac arrest management from a protocol-driven sequence into a diagnostic puzzle that, when solved, directly impacts survival.
1. Tension Pneumothorax: Emergency Decompression for Respiratory Collapse
A Tension Pneumothorax, a grave medical emergency demanding immediate intervention. This condition occurs when air accumulates in the pleural space, typically between the lung and chest wall, and becomes trapped, causing increasing pressure that collapses the lung and shifts mediastinal structures, including the heart and great vessels. Common culprits include blunt or penetrating chest trauma, which can tear lung tissue, or complications arising from mechanical ventilation, such as barotrauma. In some unfortunate instances, it can even be iatrogenic, meaning it’s an inadvertent result of medical procedures during resuscitation. Clinical signs are often dramatic and include unequal breath sounds, where one side of the chest sounds diminished or absent, a hallmark sign of Jugular Venous Distention (JVD) due to impaired venous return to the heart, and in late stages, tracheal deviation away from the affected side. Critically, patients will often exhibit severe difficulty ventilating, requiring high pressures to deliver breaths. Emergency treatment is swift and life-saving: needle thoracostomy, often performed with a large-bore needle in the second intercostal space, anterior midclavicular line, to decompress the trapped air, followed by definitive chest tube placement. Immediate recognition and decompression are paramount to avert circulatory collapse.
2. Tamponade: Cardiac Compression and Pericardial Drainage
Tamponade, or Cardiac Tamponade, is a perilous condition characterized by the accumulation of fluid in the pericardial space, the sac surrounding the heart. This fluid, whether blood, pus, or effusions, compresses the heart, preventing its chambers from filling properly, thereby drastically reducing cardiac output. Various causes can lead to cardiac tamponade, including trauma, malignancy, uremia, and infections. The classic presentation, often referred to as Beck’s Triad, includes elevated Jugular Venous Distention (JVD) due to impaired filling of the right atrium, hypotension resulting from the restricted cardiac output, and muffled heart sounds, as the fluid surrounding the heart dampens the normal sounds. Treatment is critically time-sensitive and primarily involves pericardiocentesis, a procedure where a needle is inserted into the pericardial sac to drain the excess fluid. In certain cases, especially those related to trauma or where pericardiocentesis is unsuccessful, emergency surgical intervention may be necessary to relieve the pressure and address the underlying cause.
3. Toxins: Poisoning and Overdose Management in Cardiac Arrest
Toxins, or poisoning, represent another significant reversible cause of cardiac arrest. Drug overdoses are a common scenario, with various substances having profound cardiotoxic effects that can lead to arrhythmias, profound hypotension, and ultimately, cardiac arrest. Common cardiotoxic substances include tricyclic antidepressants, known for their anticholinergic and quinidine-like effects on the heart, calcium channel blockers and beta-blockers, which can severely depress myocardial contractility and heart rate, and digitalis, which can cause life-threatening arrhythmias. Treatment strategies are highly specific to the toxin involved. When available, specific antidotes, such as naloxone for opioid overdose or glucagon for beta-blocker toxicity, are crucial. Supportive care measures, including aggressive fluid resuscitation and vasopressors, are also vital. Considerations for activated charcoal may be made in early presentations of ingestions, and in severe, refractory cases, extracorporeal treatments like hemodialysis or extracorporeal membrane oxygenation (ECMO) might be necessary to remove the toxin from the bloodstream and support organ function.
4. Coronary Thrombosis: Acute Myocardial Infarction and Reperfusion Strategies
The fourth T is Coronary Thrombosis, commonly known as a myocardial infarction (MI) or heart attack. This life-threatening event occurs when a blood clot blocks a coronary artery, severely depriving a portion of the heart muscle of oxygen and nutrients. This occlusion can lead to myocardial ischemia, injury, and ultimately, necrosis of heart tissue. Recognizing acute coronary syndrome (ACS), which often precedes a full-blown MI, is crucial. Symptoms can vary but commonly include crushing chest pain, shortness of breath, radiating pain to the arm or jaw, and diaphoresis. In the context of cardiac arrest, coronary thrombosis is a leading cause. Emergency reperfusion strategies, such as percutaneous coronary intervention (PCI), which involves threading a catheter through the blockage to open the artery, or thrombolytic therapy (clot-busting drugs) administered intravenously, are the cornerstones of treatment to restore blood flow to the heart muscle as quickly as possible. The goal is to minimize myocardial damage and improve the chances of survival and recovery.
5. Pulmonary Thrombosis: Massive Pulmonary Embolism and Thrombolytic Therapy
The fifth and final T is Pulmonary Thrombosis, or Pulmonary Embolism (PE). This severe condition arises when a blood clot, most frequently originating in the deep veins of the legs (deep vein thrombosis or DVT), dislodges and travels through the bloodstream to the lungs, where it obstructs the pulmonary arteries. A massive PE can lead to sudden cardiac arrest due to acute right heart failure, as the right ventricle struggles to pump blood against the increased resistance in the pulmonary vasculature, leading to profound circulatory collapse. Risk factors for PE are numerous and include prolonged immobility, recent surgery, cancer, pregnancy, and certain genetic clotting disorders. Clinical presentation can be non-specific, but sudden onset dyspnea, chest pain, and syncope are common. In the context of cardiac arrest, especially PEA, a massive PE should always be considered. Treatment involves immediate administration of thrombolytics to dissolve the clot and restore pulmonary blood flow. In select cases, particularly when thrombolytics are contraindicated or ineffective, surgical embolectomy to remove the clot or catheter-directed interventions may be considered to salvage the patient’s life.
Clinical Integration: Implementing the 5 Ts in ACLS Protocols
Clinical application of the 5 T’s during ACLS is not a sequential checklist but rather a simultaneous assessment woven into the fabric of resuscitation protocols. During a cardiac arrest, while high-quality chest compressions and early defibrillation are ongoing, healthcare providers must also rapidly assess for potential reversible causes. This integration with ACLS algorithms ensures that while basic life support is maintained, efforts are also directed at treating the underlying etiology. The time-sensitive nature of recognizing and treating these conditions cannot be overstated; delays can be catastrophic. A team-based approach to evaluation is crucial, with various members of the resuscitation team simultaneously performing rapid bedside assessments, reviewing patient history, and considering diagnostic possibilities.
Assessment and Diagnostic Considerations: Balancing Speed with Accuracy
Assessment and diagnostic considerations during ACLS involve a delicate balance between speed and accuracy. Rapid bedside assessment techniques are paramount. Point-of-care ultrasound (POCUS) has become an invaluable tool in identifying several of the T’s quickly at the bedside, such as cardiac tamponade (pericardial effusion), tension pneumothorax (absence of lung sliding), and even signs of massive pulmonary embolism. While less immediate, certain laboratory tests may help identify causes, such as toxicology screens for suspected poisonings or D-dimer levels for suspected PE, though these often take time to return. The challenge lies in balancing a thorough diagnostic workup with ongoing resuscitation efforts, ensuring that essential life-saving interventions are not delayed.
Treatment Priorities: Simultaneous Resuscitation and Cause-Specific Management
Treatment priorities and protocols for the 5 T’s emphasize a simultaneous approach. CPR continuation remains non-negotiable while reversible causes are being addressed. For each T, specific medication considerations might be warranted, such as antidotes for toxins or vasopressors to support blood pressure in tamponade. Surgical interventions, though less common during active resuscitation, may become necessary for conditions like severe trauma leading to tamponade or refractory tension pneumothorax. The overarching principle is to integrate these targeted treatments seamlessly into the ongoing resuscitation, optimizing the patient’s chance of survival.
Conclusion: Mastering the 5 Ts Saves Lives
The 5 Ts of cardiac arrest represent more than medical terminology – they are life-saving interventions that can mean the difference between successful resuscitation and tragic loss. Tension pneumothorax, tamponade, toxins, coronary thrombosis, and pulmonary thrombosis are reversible causes that, when rapidly identified and properly treated, dramatically improve patient outcomes. Healthcare providers must integrate these assessments seamlessly into ACLS protocols, maintaining high-quality CPR while simultaneously evaluating for underlying causes.
The complexity of cardiac arrest management demands comprehensive training, regular practice, and continuous education. Point-of-care ultrasound, rapid diagnostic techniques, and team-based approaches are essential tools in the modern emergency medicine arsenal. Remember, every second counts during cardiac arrest, and your ability to quickly recognize and treat these reversible causes can restore circulation and save lives.
Take Action: Advance Your Emergency Medicine Skills
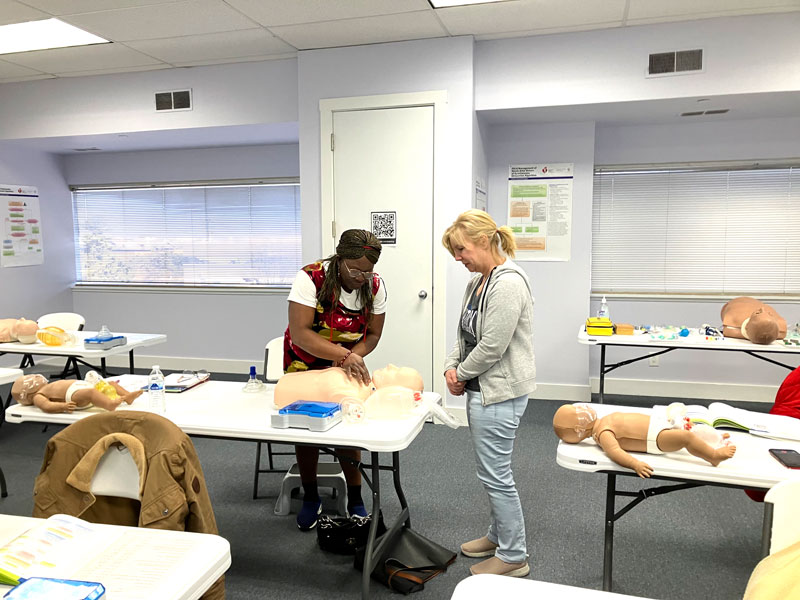
Ready to master life-saving techniques? CPR Cincinnati is an American Heart Association training site offering comprehensive CPR certification Cincinnati and ACLS certification Cincinnati programs. Our stress-free, hands-on classes cover BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid courses. As the Best CPR in Cincinnati, we provide both initial certifications and renewals to ensure you’re prepared for any emergency. Don’t wait – enroll today and become the healthcare hero your community needs.